Things have changed rapidly as a result of COVID-19 and a few trends that will emerge out of this situation will become drivers of transformation in the future. Providers will rethink their capacity and the ways in which they are providing care. Going completely virtual can lack empathy as we are all social and we need conversations rather than just transactions – especially when it comes to our health. One bold prediction is that patient access centers will emerge as a new form of caregiver rather than just care providers. They will bridge the clinical world asks with patients via an empathetic dialogue.
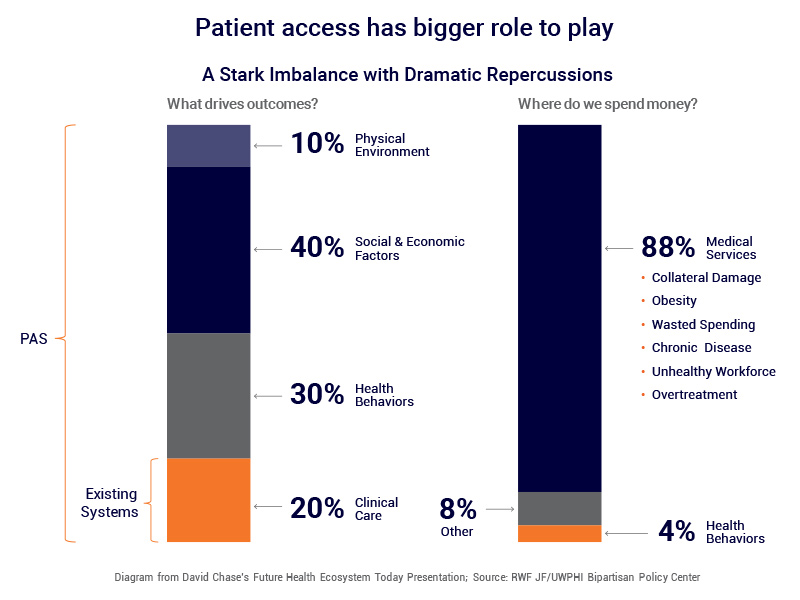
In a recent study from RWJ suggests that, what keeps us healthy are more dependent on social and economic factors that shape behavior, more so than clinical procedures and drugs. Preventative Medicine is the mantra but look where healthcare spending continues to be focused. The current technical infrastructure like EMRs only supports clinical care and there is no mechanism in these systems to influence health behavior or manage social-economic factors which in turn impact an individuals’ life and their health.
Accordingly, the entire health system is fundamentally changing the way they are operating by focusing on keeping the individual healthier outside vs. bringing them into hospitals for care. It’s not easy and that’s where patient access services will step in. They will need to be more outbound and proactive rather than just reactive and addressing inbound requests.
Essentially, the industry is looking at patient access and engagement as a linchpin for balancing patient health as well as hospital operations and revenue. Providers will be focused on how improved patient access will deliver value to the hospital system by increasing the use of patient panels, engaging patients in their care plan, and managing network integrity. The expected results will include increased utilization volume, incremental revenue by maximizing providers productivity, expanding practice capacity and driving downstream referrals. All of these will be managed by Patient Access Centers.
Along with managing patient dialogs empathetically and proactively, Patient Access Centers will be included in strategic operational conversations addressing the following points:
Improving Patient Engagement
- Poor management of scheduling model results in extremely long wait times
- Misalignment of scheduling model results in significant ‘referral leakage’ thus a significant loss in annual revenue
Increasing Provider Capacity
- Reducing loss of capacity & revenue due to high no-show rates
- Enabling providers to work at top of their license – 7 hours weekly of cFTE capacity missing in practices
A software-driven Patient Access Center of the future will address:
- Physician’s Global Availability: Challenging to find first available slot across the system
- Multiple Systems: (Multiple EMRs, billing systems, scheduling systems, etc.) Multiple Transfers, teams limited to their locations
- Patient Amnesia: Same questions for each new transferred call
- Previous Patient Interaction Tracking: No traces, No patient view, Patients call back for reminders
- Billing Challenges: Multiple Unstructured Documents, No Unified Timeline, Complex Triaging (Payer, Patient, Billing staff), Technology Performance (Credit Card Payment)
- Patient 360 View: Having a comprehensive view of all patient interactions, communication, and requests