Authors- Dr. Sawad Thotathil (Sr. Director – Digital Health), Swapnil Paranjpe (Sr. Director – Digital Solutions)
Increasing patient access to healthcare has always been of prime concern to health systems. In a fee for service world the need to increase patient volumes was a key driver for enhancing access to care. However, capacity challenges often lead to closed patient panels or long waiting times. This problem continues to worsen and waiting times continue to rise. According to a recent Merritt Hawkins survey (1) patients in many of the large metro markets are experiencing average new patient physician appointment wait times of 14 days or longer. It was also observed that the average physician appointment wait times in the 15 large metro markets have increased significantly over similar wait times tracked by the survey in 2014, 2009 and 2004. Refer to detailed analysis based on the survey conducted by Merritt Hawkins.
It is important to note that waiting time to appointment is only one objective measure of access to care in a community. Other metrics include same day availability, extended (beyond office hours) availability and several others which are being tracked by institutions across the country. Most of these metrics reflect both capacity as well as policy and processes at these organizations. Pressure to improvise had been limited until more recent years but patient expectations have significantly changed and patient access to care has become a key strategy in responding to the demands of a value based care economy. Let us look at these changing demands more closely and how health systems could enhance access to care.
Patient-Provider Relationship and the experience of care
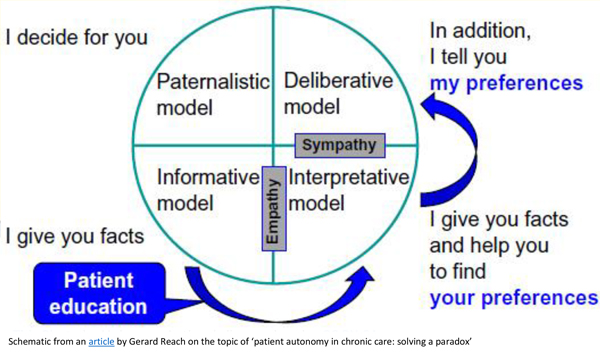
Patient preferences are changing. Their expectations are being increasingly shaped by the experiences in retail outlets and online stores but there is no doubt that healthcare is different. It is a dysfunctional market due to the inherent information inequality between provider and patient; but there are several arenas where patients can make choices as they would in most other parts of their life. Below schematic provides us a good overview of the likely spectrum of patient autonomy with preferences and corresponding patient-physician relationship. But, eventually it will be largely up to the provider to determine the boundaries of this autonomy, largely based on the clinical scenario and impact of the preferences on the clinical outcome.
Reference – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865080/figure/f2-ppa-8-015/
Price and quality are 2 obvious dimensions of care where patients do believe choices can be made given enough information. Cost transparency is a well know challenge and there are attempts by startup companies trying to provide patients with price estimates despite the inability to discern any logical mechanism pertaining to the hospital charge master.
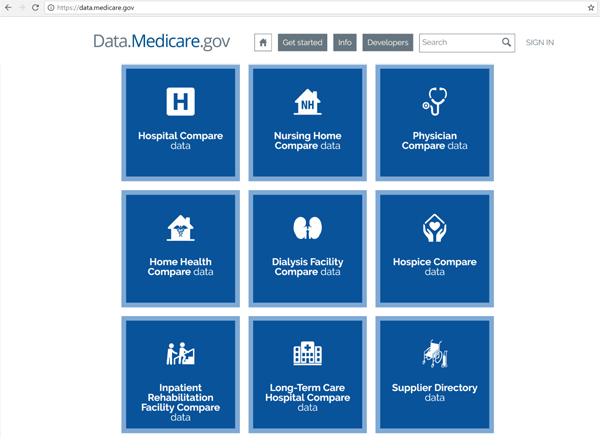
Quality is an even more complicated arena. While dissemination of quality information is happening, as in quality metrics publicly available in Hospital Compare, the ability to make choices based on those numbers is hampered by the fact that these clinical quality metrics never factor in the differences in patient types between hospitals. As an example, it is an unfair comparison when an academic hospital tending to the most complex and complicated patients are compared with smaller community hospitals which by their very nature tend not to handle the most complex cases. Regardless, most patients find these publicly reported measures difficult to understand when trying to make choices.
Reference – https://data.medicare.gov/
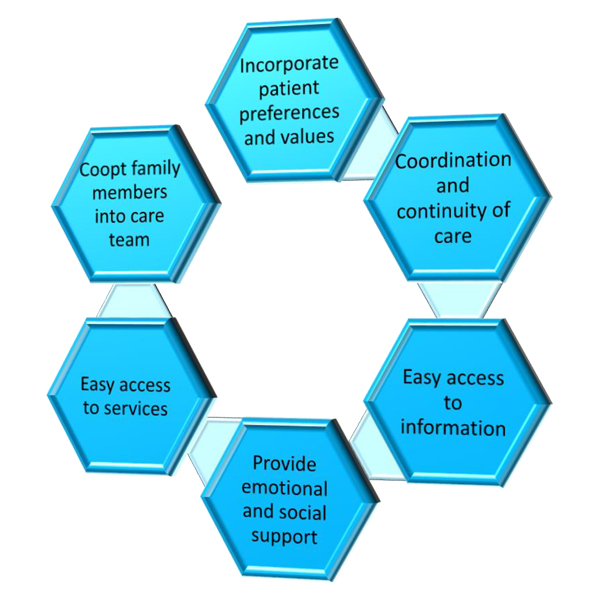
However, quality includes the total experience of the patient, and beyond clinical metrics, there are hospitality and operational factors which have a big influence on how patients perceive quality. These 2 arenas are not just easily perceived by patients but are also amenable to measurement in a way that is understandable by the patient. The steady transition of healthcare organizations’ business model from fee-for-service to a value based model is impacting the drive toward improving this experience while increasing clinical quality and reducing costs. These 3 goals are inter-related and access to care becomes the key link between the 3. Pro-active approaches to provide information, guidance and support to patient when they need it and where they need it can help patients remain safe and stable in their preferred environments minimizing the need to rush to the emergency room or acute services. Patient centeredness thus becomes the central strategy in value based care.
Challenges to Patient Centeredness
Implementing Patient centeredness comes with its challenges and it is important to point out 3 of the main ones
- As the goal is to reduce use of acute services through pro-active reach to patients in need, this necessitates a ramping up of services in the community. This comes up against a capacity issue confronting many health systems. Shortages in primary care clinicians are magnified by the fact that the demographic trends – ageing – and disease patterns – more chronic disease load – are on the rise.
- Providing convenience to patients through easier access has the unintended consequence of increased utilization. Research from direct to consumer telehealth has shown that new utilization is real consequence and so strategies for patient access must have a more comprehensive approach to new service provision and resource allocation across the system to mitigate the risks of new utilization.
- Clinical Research and the ability to do biomedical research are accelerated because of increased computing power. This has the positive effect of increased data about patients and more effective ways to respond to them. Genomics and social data are key enhances in this changing data environment. However increased data becomes a challenge for organizations that already do not have effective approaches to consolidate patient data and use it for operational effectiveness.
Any strategy to achieve patient centeredness thus has to overcome these challenges and we believe there is a powerful tactical approach to do this. The common link between achieving comprehensive without over-utilization, rationalizing allocation of resources and the data deluge is to create a system that profiles the patient more precisely. The enormous quantity and types of data need to do this is a technical and organizational challenge. The picture below illustrates well the numerous “layers” of data that help a provider understand better the patient better. Understanding the patient better helps match the organization’s resources more precisely to their needs. A more precise approach to responding to their needs allows more careful allocation of resources and better control over the consequences of care provision.
Reference http://www.cell.com/cell/fulltext/S0092-8674(14)00204-9
There is however another major category of data that captures the patient’s life story and that will go a long way in matching the patient’s needs to what can be offered. A lot of unstructured information about the patient is documented in clinical notes and logs of communications with patients. Making sense of this data and inserting these insights into provider workflows and decision making will go a long way in improving experience and quality of care. Let us look at how cognitive search technologies can help providers create value from this kind of data and how such tools help enhance patient centeredness in care delivery.
Relevance of Cognitive Search in Improving Patient Access
Cognitive Search is a sophisticated and natural technique to deliver pertinent information to users and is actionable. It seeks to derive user intent based on the user traits, interaction and behavior, combined with understanding of what information other users of similar kind have found useful.
Cognitive Search delivers through several dimensions that will work together to provide desired outcome, and more importantly will keep learning to refine based on new data related to user activities.
A few examples will clarify whether a certain cognitive play is working or not. For e.g., in case of ambiguous input, instead of waiting for a correction from the user or keeping the user guessing, cognitive search will seek to decipher based on what the machine knows about the user (profile, role, context, relation, etc) and its surroundings and making practical input deviation that closely fits the model.
This also leads to conversational information discovery, ensuring the user a more cerebral pathway.
Another example is of the machine providing guided navigation or personalized recommendations based on trait profile that machine has built about a particular user and then extracting what information has been found useful or approved by others with similar traits. And, this model is never static or constant and will adapt to changing preferences of the group.
I also call Cognitive search as Empathic search, in the sense that before providing a response or information or direction, the system will pursue to comprehend expectation and purpose of the user.
In context of the patient centeredness and access, Cognitive search offers to help those who care for the patient by combining, dissecting and correlating the information about the patient, her diagnosis and care needs with the knowledge siloed within the health center and in the public medical domain, and contextualize and personalize for that particular patient. An article by Dr. Gordon Jones on patient access modernization calls out, among many other factors, importance of patient information leverage, patient self-service, delivering intelligent insights and access unification – to achieve the goal of patient centeredness.
Cognitive search can do this without sacrificing the fundamental issues of data security and privacy, ensuring that individual attributes, traits and other currency values associated with the patient are not exposed to anyone who is not authorized or intended to access that information.
Advisory firms like Forrester Research strongly recommend businesses to consider cognitive search to transform their business.
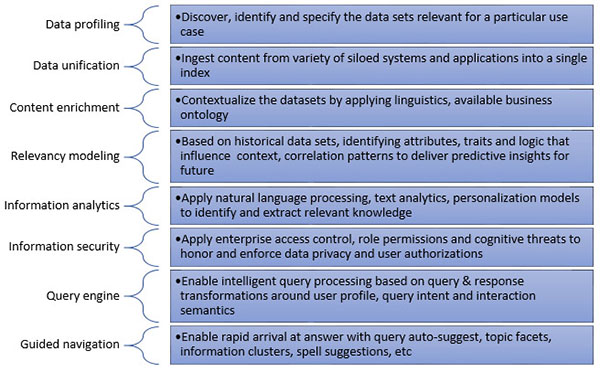
Cognitive search involves several steps before the data is transformed into meaningful information and useful knowledge, of which we list a few important ones here –
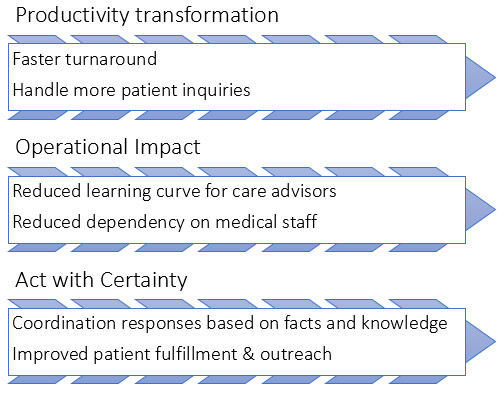
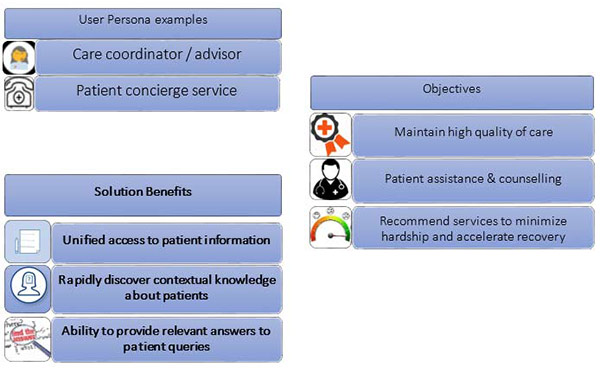
Modern platforms such as Attivio Cognitive Search and Insight offer such technical capabilities and make it possible for healthcare providers to rollout intelligent solutions that make patient engagement transformations real and now. As an example, we illustrate below how within a patient concierge management or care coordination program, the technology allows quick access information relevant to the patient and make recommendations at minimal overhead.
We further illustrate how cognitive search capabilities will benefit specific healthcare role.
It is our belief that Cognitive search applied towards patient care and access to services can be a big step forward in assisting the providers in their move toward creating more value for patients.
For Salesforce based healthcare businesses, Persistent Systems is offering Engage 360 solution on Service Cloud for enabling Healthcare enterprises with delivery of patient access and centeredness solutions aligned with their care coordination goals and infrastructure specifics.